A person with obsessive compulsive disorder (OCD) experiences intrusive, unwanted and uncontrollable thoughts or mental images (obsessions). To reduce the anxiety caused by these thoughts they engage in repetitive actions or behaviours (compulsions). These obsessions and compulsions are distressing and cause extreme disruption to everyday life. The types of obsessions and compulsions experienced and the severity of these symptoms can change over time and may be triggered by stress.
Obsessions and compulsions are linked. A person with OCD feels they need to perform these repetitive behaviours or actions to reduce the anxiety and distress caused by the thoughts. Common compulsions include repeatedly checking things, counting, tapping, or washing your hands for longer than or more than needed. Once these behaviours are complete the anxiety reduces. However, these thoughts and images occur again and again, and the behaviours and anxiety continue to increase over time.
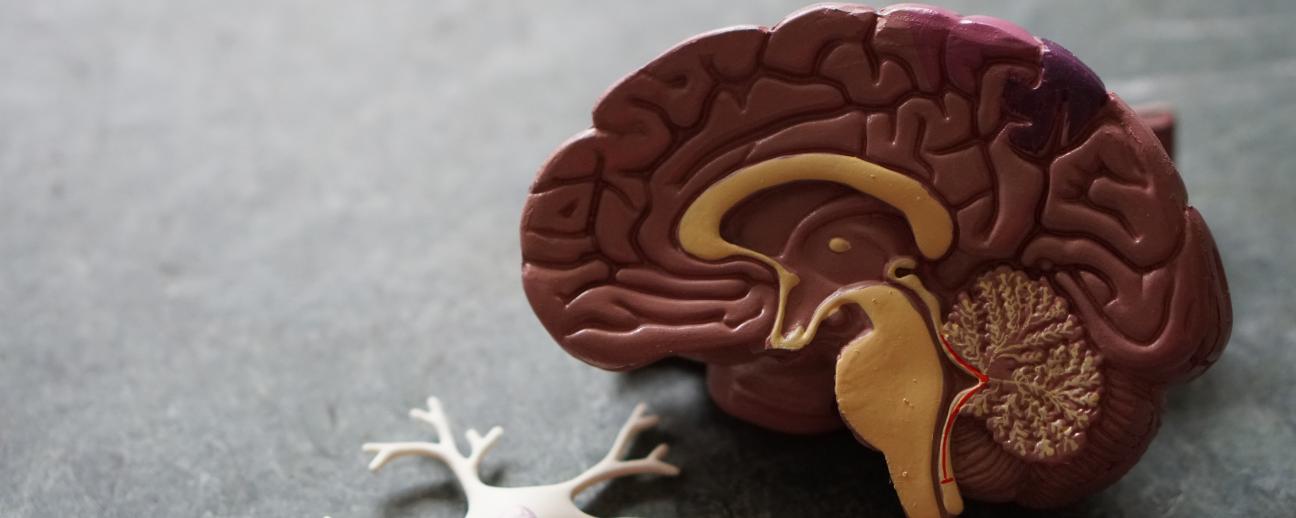
Risk factors in the development of OCD include a family history of OCD, experiencing a stressful life event, and the presence of other mental health disorders. There is also growing evidence that in those with OCD there are physical changes in areas of the brain involved in controlling thoughts and actions.
- Persistent, intrusive, unwanted thoughts and mental images that lead you to perform repetitive behaviours.
- Feeling that you need to engage in the behaviour to stop these thoughts/ mental images.
- Obsessions and/or compulsions take up excessive amounts of time - more than 1 hour per day.
- Obsessions and/or compulsions interfere with daily routines and cause significant distress. E.g. they have a negative impact on school/ work/ relationships.
- Trying to ignore the thoughts or stop the behaviours increases anxiety and distress.
- Performing the behaviours/ compulsive acts reduces anxiety and stress.
- Difficulty sleeping
- Low mood
- Feeling anxious
- Panic attacks - sudden intense fear and anxiety causing physical anxiety symptoms.
- Thoughts of harming yourself
- Thoughts of suicide or death
OCD is commonly treated with a combination of psychological therapy and medication. Although treatment may not cure OCD, it can successfully reduce the symptoms and the distress and anxiety caused by these symptoms. Seeking help early can lead to better outcomes, so if you think you have OCD it is important to speak with your doctor.
Psychological Therapy:
Exposure and response prevention (ERP) therapy and cognitive behavioural therapy (CBT) are common psychological therapies used to treat OCD.
ERP therapy is a form of behavioural therapy in which the individual is gradually exposed to situations that cause obsessions and anxiety. The aim of ERP is to teach coping skills to help control compulsions and reduce anxiety when these thoughts and mental images are experienced.
CBT is a structured form of talk therapy which combines cognitive and behaviour therapies. CBT for OCD aims to change the way you respond to the thoughts and mental images (obsessions) and teach coping strategies to reduce distress and anxiety.
Medication:
Antidepressants are commonly prescribed in the treatment of OCD to help reduce intrusive thoughts and anxiety, control compulsions, and improve mood. You may need to trial several types and different doses of medication with your doctor to find one that is effective for you.
Other Treatments:
Transcranial magnetic stimulation (TMS) may be used to treat adults with OCD who have not had success with psychological therapy and medication. During TMS an electromagnetic coil is placed on the head and short magnetic pulses are sent into particular areas of the brain. This aims to stimulate nerve cells to reduce symptoms.
Those who are experiencing severe OCD which is having a major impact on their daily functioning may require residential treatment or a more intensive outpatient treatment programme.
Other Ways to Manage OCD:
Joining a support group and talking to others about their experience with OCD can be helpful.
Meditation, deep breathing, progressive muscle relaxation, and other relaxation techniques can help to reduce general anxiety and stress.
It is also important to look after your general physical and mental health by maintaining a healthy lifestyle. Stay physically active, eat a healthy balanced diet, get good sleep, and find hobbies you enjoy.
The OCD NZ website provides resources and information on OCD to help those living with OCD or supporting people with OCD. The website provides information about the condition, where to seek help, the types of treatment available, and provides a great list of resources, such as books, organisations, and other websites.
Fixate is a New Zealand OCD support group. It is a Facebook page which provides a space for those living with OCD or supporting someone with OCD. This Facebook page is a place for discussion, posting helpful resources, and is a way to connect with others going through a similar experience.
OCD Action is a UK OCD charity. They aim to provide information and support to those living with OCD and to raise awareness about the condition. The OCD Action website provides helpful information about OCD, treatment options, and ways to access support.
Anxiety NZ Trust is a non-profit, registered charity who support kiwis suffering from OCD, anxiety, and other anxiety related disorders. Their aim is to raise awareness and to provide support for those living with these conditions. They run workshops and support groups, and provide education and treatment. Anxiety NZ also have a 24/7 free confidential national anxiety helpline (0800 269 4389).
The international OCD Foundation (IOCDF) works to help those living with OCD by increasing access to treatment, providing resources and education, raising awareness, and fighting stigmas surrounding OCD. Their website contains great information on OCD, treatment, and links to other useful resources.
The OCD Stories is a free weekly podcast which aims to raise awareness and provide education on OCD. Episodes contain interviews with therapists, psychologists, researchers, and those living with OCD who share their personal stories and experiences.
OCD is a serious mental health condition, yet it is often misunderstood. This TED-Ed video addresses some of the misconceptions surrounding OCD.